DR. MED. ANDREAS KRÜGER (MD, POLODOC)
Specialist in Orthopaedic Surgery and Traumatology FMH
Hamstring Injuries
The hamstring comprises most of the muscle bulk in the back of the thigh. It is important for pushing off, jumping and landing and especially when riding for ensuring good contact to the saddle. The hamstring is made up of three muscles - the biceps femoris, the semitendinosus and the semimembranosus, each with a common proximal attachment via a large tendon to the ischial tuberosity of the pelvis (the large bone you sits on in the buttock).
Hamstring Injuries: High energy and extension issues
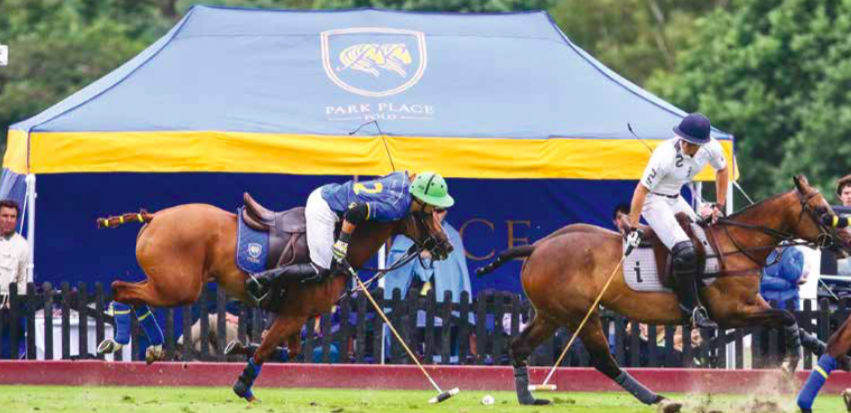
A powerful eccentric contraction can injure the hamstring tendon when extending too far out of the saddle
(Andreas Krüger MD @polotimes.co.uk)
The hamstring comprises most of the muscle bulk in the back of the thigh. It is important for pushing off, jumping and landing and especially when riding for ensuring good contact to the saddle. The hamstring is made up of three muscles - the biceps femoris, the semitendinosus and the semimembranosus, each with a common proximal attachment via a large tendon to the ischial tuberosity of the pelvis (the large bone you sits on in the buttock). This proximal attachment provides a fixed point from which muscle contraction can affect a more distal action - the hamstring provides some hip extension, but the main action is movement around the knee. This is the main muscle group responsible for knee flexion. The sciatic nerve runs very close to the proximal tendon attachment to the ischium and can be injured together with the hamstring.
mechanism of injury
Powerful eccentric contraction, i.e. not placed centrally, either injures the proximal hamstring tendon through a progressive stretch or more commonly, when the hip is suddenly and forcefully flexed over an extended knee. This happens when you try to stay in the saddle while falling and the horse adds an additional opposite force. Proximal hamstring injuries can be complete tendon ruptures or incomplete/ partial tears. In a young person, the bone with the tendon attached is often separated or fractured from the pelvis (ischium).
Presentation of a hamstring injury
The rider will feel something 'go', deep in the buttock. If the incident is observed by others, often the player will grab the buttock or upper thigh - the so called 'clutch' sign of a hamstring injury. They are generally not able to continue with activity and if on the ground may need assistance to get up and walk. There is usually immediate pain and weight bearing on the affected leg is very difficult, so crutches are usually required. It is painful to sit on the affected buttock. Over the next 24 to 48 hours there is usually swelling and bruising that appears over the buttock area, which then extends down the back of the thigh and sometimes even into the lower leg. Occasionally there can be pins and needles in the foot or lower leg and loss of movement in the foot can be seen with a foot drop in rare cases.
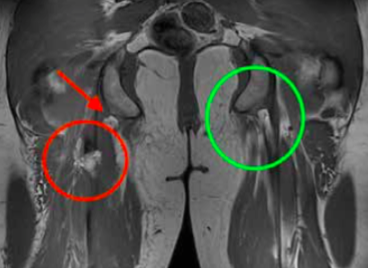
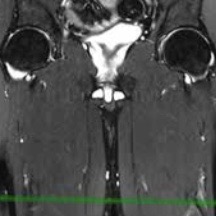
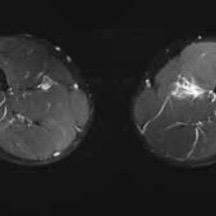
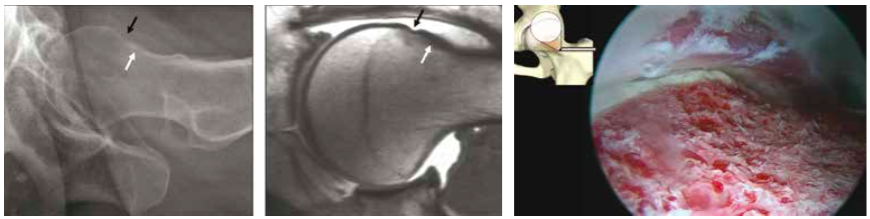
An MRI is the gold standard for identifying hamstring tendon tears. The red circle signifies an injured tendon, whereas the green circle shows a healthy tendon.
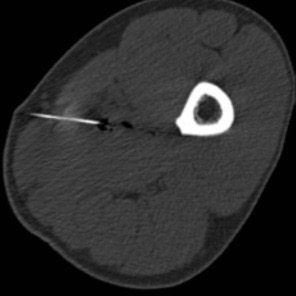
Investigation: X-rays
X-rays are important for younger patients, to rule out a fracture of the bony attachment.
Ultrasound
Ultrasound can identify a blood collection in the buttock and upper thigh, whilst also detecting tendon tears.
MRI
An MRI scan is the gold standard which is highly accurate at determining the site of injury, whether the tear is partial or complete and importantly whether there has been any retraction of the tendon end into the thigh.
A powerful eccentric contraction can injure the hamstring tendon when extending too far out of the saddle (Photography by imagesofpolo.com)
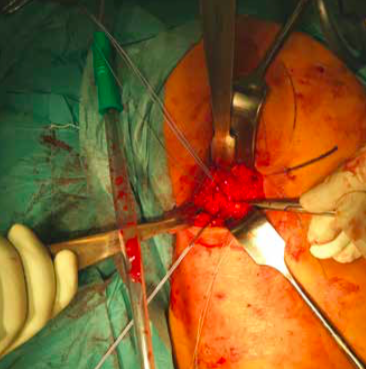
Operative repair of a hamstring tendon is recommended when there is a complete tear
The incision is made in the buttock/upper thigh area where the torn tendon end will be found
Treatment
Initial treatment in the first few days should be symptomatic - measures to reduce pain and swelling with icing, analgesia and the use of crutches to assist walking. As the pain starts to settle, some gentle movement of the leg can be beneficial and the assistance of a physiotherapist at this point can be very helpful.
Once the diagnosis of a hamstring injury is made, it is important to get a specialist opinion regarding treatment options. Conservative treatment with a rehab programme may be appropriate for players with a low demand, or those with partial tendon tears where a significant proportion of the tendon is still intact. Operative repair of the tendon is generally recommended when there is a complete tendon tear. Surgical repair usually involves an overnight stay in hospital and the procedure itself is performed under general anaesthetic. An incision is made in the buttock/upper thigh and the torn tendon end is identified, mobilised if it is retracted down into the thigh and then repaired back onto the bone using bone anchor sutures.
Rehabilitation
After surgery, painkillers are generally required. Post-operation, a positioning pillow under the knees will relax the hamstring and a leg brace will control the degree of extension. Initially the knee will be limited to a 60 degree flexion. A systematic progression of extension is advised in two-week intervals, increasing the extension in 20 degree steps. Crutches will be needed for six weeks, putting a small amount of weight on the ground and the extension of the knee is limited with a brace. At six weeks, patients will start loading of the leg with possibly a return to light running and soft riding at three to four months. A return to chukkas may be considered after six months.
Physiotherapy protocol
(by Gregor Schwarzer, Gsports.ch)
It is important to know how the region of the lower back/pelvis/ hip is put together. The physiotherapy programme following surgery will be divided in four periods of time:
period one
Day 0 to 5: Vascular and cellular phase with inflammation control. This is the healing phase of the skin and the soft tissue underneath. It is essential to control inflammation of the vascular and cellular phase.
period two
Day 5 to 20: Proliferation. The healing from Period One will continue while a scar is created on the surface.
period three
Day 21 to 60: Consolidation of work. The wound's scar tissue should be stable by this point, so the rehabilitation is now about consolidation.
period four
Day 60 and onwards: Organisation and reconstruction (the most important element).
The adequate stimulus of the tendon matrix is the most crucial element when finding the way back to full function, following a strict regime according to the aforementioned periods.
Rehabilitation
Day 1 to 21: Local therapy is required. Start with lumbar spine treatment as well as treatment to the hip/leg region. Day 21 to 42: Testing the trunk musculature and control of the body's symmetries. Day 42 onwards: Begin your return to activity while undertaking quality exercises. To regain your former activity level will be challenging.
For more information contact Andreas Krüger MD
Andreas Krüger is a Swiss board orthopaedic and trauma surgeon in Zurich, who specialises in knee and shoulder surgery. Andi is a second generation of tournament doctors for equine sports, known as Polodoc since 2013 and is a member at Legacy Polo Club in Switzerland
Sports medicine and orthopaedic surgery
Dr. med. Andreas Krüger is a specialist in orthopaedic surgery and traumatology of the musculoskeletal system and supports both hobby athletes and global top athletes. He is one of the leading specialists in the field of regeneration after training and competition and is a key-operation leader in the fields of polo and sports medicine and surgery.
Dr. med. Andreas Krüger is a specialist in orthopaedic surgery and traumatology of the musculoskeletal system and supports both hobby athletes and global top athletes. He is one of the leading specialists in the field of regeneration after training and competition and is a key-operation leader in the fields of polo and sports medicine and surgery.
Source: patientube.com
Andreas Krüger (PoloDoc)
Andreas Krüger is a Swiss board orthopaedic and trauma surgeon in Zurich, who specialises in knee and shoulder surgery. Andi is a second generation of tournament doctors for equine sports, known as Polodoc since 2013 and is a member at Legacy Polo Club in Switzerland.
Specialist in Orthopaedic Surgery and Traumatology FMH
Patientube: Interview with Dr. med. Andreas Krüger
Dr. phil. Dr. med. Anna Erat (patientube_com) in an interview with Dr. med. Andreas (PoloDoc)
patientube_com Interview: Dr. phil. Dr. med. Anna Erat and Dr. med. Andreas Krüger #andreaskrüger #annaerat #patientube #unalone #polo #polomatch #polodoc #andikrüger
Andreas Krüger (Sports Medicine and Knee Surgery)
Polo injuries - need an orthopaedic surgeon?
In the world wide web you will find only rare articles about polo injuries. One of these scientific articles concludes that at every tournament an orthopedic and trauma surgeon should be present at all times.
In the world wide web you will find only rare articles about polo injuries. One of these scientific articles concludes that at every tournament an orthopedic and trauma surgeon should be present at all times.
Protect Your Muscles
The most common cause of groin pain is a muscle, tendon or ligament strain, especially in athletes who play stop and go sports. Groin pain might occur immediately after an injury, or pain may come on gradually over a period of weeks or even months and will be worsened by continued use of the injured area. Less commonly, a bone injury or fracture, a hernia or even kidney stones might cause groin pain. Although testicle pain and groin pain are different, a testicle condition can sometimes cause pain that spreads to the groin area.
Tune up the brakes - Optimise the muscle
(Dr. med. Andreas Krüger @polotimes.co.uk) Polodoc Medical Insight September 2017
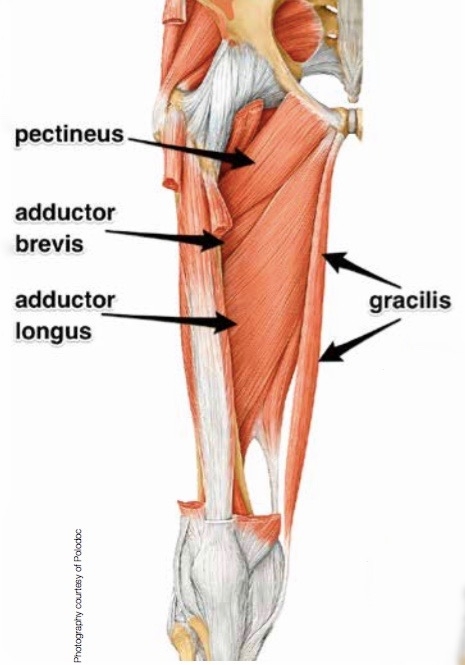
Stopping the horse and keeping the position in the saddle while changing direction can create extreme tension to the thigh musculature. This peak tension can damage a cold or not prepared muscle. A strain, muscle pull, or even a muscle tear refers to damage to a muscle or its attaching tendons. You can put undue pressure on muscles during normal riding, normal daily activities, with sudden heavy lifting, during sports, or while performing work tasks.
Injury pattern
Muscle damage can be in the form of tearing (part or all) of the muscle bres and the tendons attached to the muscle. The tearing of the muscle can also damage small blood vessels, causing local bleeding, or bruising and pain caused by irritation of the nerve endings in the area. Typical injury happens when the player is not warmed up and pre-riding stretching was left out, in particular, the half seat and braking, needs maximum contraction of the adductor muscles.
Symptoms of muscle strain
Swelling, bruising, or redness due to the injury
Pain at rest
Pain when the speci c muscle or the joint in relation to that muscle is used
Weakness of the muscle or tendons
Inability to use the muscle at all
Diagnosis
In most of the cases, the injury history, the injury pattern and clinical examination help to ne the diagnosis.
first line treatment
The muscle pattern of the upper thigh and adductor
Protect the strained muscle from further injury and rest the strained muscle. Avoid the activities which caused the strain and other painful activities. Ice the muscle area (20 minutes every hour while awake). Ice is a very effective anti-in ammatory and pain reliever. Small ice packs, such as packages of frozen vegetables or water frozen in foam coffee cups, applied to the area may help decrease in ammation. Compression can be gently applied with an Ace or other elastic bandage, which can both provide support and decrease swelling. Do not wrap tightly and elevate the injured area to decrease swelling, propping up a strained leg muscle while sitting, for example. Activities that increase muscle pain or work the affected body part are not recommended until the pain has signi cantly improved.
Professional treatment
The most important key to treatment is the early diagnostic proof of a working diagnosis from clinical examination. Ultrasound is the best form of examination where the exact point of maximum pain can be detected, while the MRI (Magnetic Resonance Imaging) is most precise in ning the extent of injury in a standardised fashion. Following this a computer tomography guided in ltration can deliver painkillers (Ketorolac) directly to the spot of the lesion with additional PRP (Platet-riched Plasma - ACP or Hyaloron Tendon) for accelerated healing. After treatment, physical workouts should be limited the frst 48 hours. A physiotherapeutic workout should consist of an eccentric training with local analgesic treatment (Ultrasound, TENS). The new Compex® SP 8.0 treatment programmes can alleviate pain, measuring the individual impulse needed to optimally stimulate the muscle. At the same time, muscle training should also be undertaken. Beyond this manual treatment, auxiliary local compression with thigh sleeves may also reduce the symptoms.
An MRI Scan can be the most useful diagnostic tool
When adequate stretching has not taken place before..
... a match, injuries to the muscles becomes more likely
return to play
The intervals between injury and a return to sport are different for each individual. After a minimum of three weeks recovery, pain free normal gait and a less than few seconds squeeze test are mandatory perquisites to go back in the saddle. In the worst cases of muscle injury, even longer periods are recommended.
Electrical stimulation can also help speed up recovery
Prevention
Most muscle injuries are due to a neglected preparation timetable for the maximum load and strain on the tissue. So, repetitive micro injuries can lead to chronic impairment. Elasticity of the muscle is key, so adequate stretching before and after the game is crucial. Optimal preparation with additional workout through electrical stimulation may also be helpful.
Stretching before and after the match is important to prevent injury
When to see your doctor
Hematoma in the region of pain
Palpable cavity in the muscle
Ongoing pain for more than one week
Rule out symphysis injury
For more information contact Andreas Krüger MD
Groin Pain and No Flexibility
The most common cause of groin pain is a muscle, tendon or ligament strain, especially in athletes who play stop and go sports. Groin pain might occur immediately after an injury, or pain may come on gradually over a period of weeks or even months and will be worsened by continued use of the injured area. Less commonly, a bone injury or fracture, a hernia or even kidney stones might cause groin pain. Although testicle pain and groin pain are different, a testicle condition can sometimes cause pain that spreads to the groin area.
Groin Pain and No Flexibility
(Dr. med. Andreas Krüger @polotimes.co.uk) Polodoc Medical Insight April 2018
A bad combination
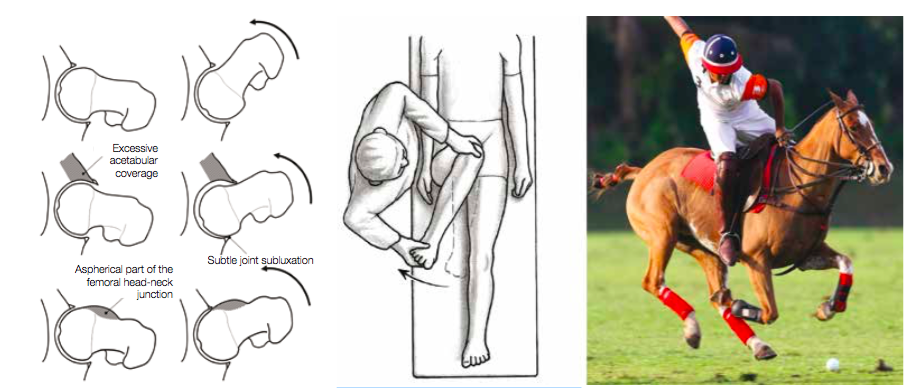
Flexibility to bend forward while standing in the stirrup and the freedom in the hip is key to reach out and win the ball in the one-to-one situation. Even while doing a regular polo swing and turning the upper part of your body, a relevant rotation in the hip is performed.
A reduced range of motion in the hip or a more relevant stiffness can lead to a pain problem limiting the performance of playing polo. The orthopaedic reason for this can be a mismatch between the ball and the socket of the hip, which is called femoral acetabular impingement (FAI).
How do I get FAI?
Some experts believe that significant athletic activity before skeletal maturity increases the risk of FAI, but no one truly knows. Sports with significant contact (i.e., football), with repetitive stress to the hip and male gender are associated with an increased likelihood of FAI.
Types of FAI
FAI generally occurs in two forms - Cam and Pincer. The Cam form describes the femoral head and neck relationship as aspherical or not perfectly round. This loss of roundness contributes to abnormal contact between the head and socket. The term Pincer (which comes from the French word meaning 'to pinch') describes the situation where the socket or acetabulum has too much coverage of the ball or femoral head. This over- coverage typically exists along the front-top rim of the socket (acetabulum) and results in the labral cartilage being 'pinched' between the rim of the socket and the anterior femoral head-neck junction. The Pincer form of the injury is typically secondary to 'retroversion', a turning back of the socket ('profunda'), a socket that is too deep ('protrusio'), or a situation where the femoral head extends into the pelvis. Most of the time, the Cam and Pincer forms exist together, otherwise known as 'mixed impingement'. FAI is associated with cartilage damage, labral tears, early hip arthritis, hyperlaxity, sports hernias and lower back pain. FAI is common in professional athletes, but also occurs in active individuals.
Prof. Dr. M. Tannast
Notes from Consulting Expert for Joint Preserving Hip Surgery Prof. Dr. M. Tannast of Bern University
1) Repetitive sports in adolescents can lead to an early onset alteration of the hip. 2) 50 percent of the cases are misdiagnosed as a 'sports hernia'. 3) The majority of problems can be solved with minor invasive surgery using arthroscopic methods.
Other reasons for groin pain
The most common cause of groin pain is a muscle, tendon or ligament strain, especially in athletes who play stop and go sports. Groin pain might occur immediately after an injury, or pain may come on gradually over a period of weeks or even months and will be worsened by continued use of the injured area. Less commonly, a bone injury or fracture, a hernia or even kidney stones might cause groin pain. Although testicle pain and groin pain are different, a testicle condition can sometimes cause pain that spreads to the groin area.
Groin pain commonly has its origins in the hip joints
The diagnosis of FAI
Patients will undergo a physical examination which will include:
The hip clinical examination should be
done with great care, because it provides the most reliable diagnostic information Physical findings will dictate further tests and necessary management.
Observation of a patient's sitting posture, gait, palpation of the hip, abductor strength testing, careful hip range-of- motion (ROM) assessment and specific provocative tests like the impingement test (rapid internal rotation of the leg in 90 degree flexion and adduction) should be performed.
Radiological examination: The investigation of FAI requires a combination of a roentgenographic examination and more sophisticated cross-sectional studies, such as magnetic resonance imaging (MRI) with performance of specific action.
Cam type FAI in a 37-year-old woman and the joint after arthroscopic treatment
Treatment of FAI
Conservative treatment Activity restriction or cessation may alleviate symptoms in some patients. Athletes involved in repetitive hip flexion activities may experience significant relief of discomfort if they refrain from their sport. Although conservative measures are likely to be temporarily successful in some patients, those with a high activity level and athletic ambitions usually have low compliance. Conservative treatment may help and should be applied as a first-line treatment in symptomatic hips, especially those with mild and intermittent symptoms, before surgery is considered. Treatment may include activity restrictions, hydrotherapy, anti-inflammatory medicines and intra-articular injections. The severity of the clinical picture will dictate the eventual therapeutic methods used. Physical therapy, emphasising the improvement of passive hip ROM, or stretching, is counterproductive and should be avoided because it will irritate the hip and subsequently worsen the pain by sustaining and evolving articular surface damage.
Surgical treatment
Surgical treatment of femoroacetabular injury focuses on improving the clearance for hip motion and alleviation of femoral support against the acetabular rim. This includes the surgical resection of the injured area, by trimming the acetabular rim or the femoral head-neck offset either via a surgical hip dislocation or arthroscopically. Mid-term results from these procedures are promising.
Use of the Racewood Horse can provide a full analysis of the seat position and swing technique, here shown at reitsimulator.ch with an equine sport therapist
Diagnostics and possible adjustments of riding technique
With the use of the Racewood Horse, a full analysis of the seat position and swing technique off the field can be performed. The medical expert can detect and correct painful positions whilst in the saddle and performing the swing. Typical intra-game problems can be simulated and analysed. The focus here
is on posture with control of muscle power and use, as well as pelvic spine coordination and maybe, if indicated, adjustments of the equipment. A complete work up of the groin pain should be performed with a treatment plan consisting of all components of conservative and if needed of operative therapy should be discussed.
Checkbox
To reduce internal rotation and groin pain, please see an orthopaedic surgeon for a consultation.
Rule out additional or other causes of injury with a sports specialist.
A full assessment of riding techniques with the help of a simulator can help to minimise future mistakes.
For more information contact Andreas Krüger MD
Special thanks to J. Landry (photographer)
Torn cruciate ligament - typical ski injury - do you always have to operate?
Torn cruciate ligament - typical ski injury - do you always have to operate? Knee injuries are the most frequent ski accidents on the slopes, accounting for about 30% of all injuries. Right at the top of the statistics is the torn cruciate ligament. There are various criteria that are taken into account when making individual decisions about treatment. But which treatment is the right one for two of my patients? Both love skiing and both injure their anterior cruciate ligament. Their stories could not be more different. Former junior skier vs. hobby skier, surgery vs. conservative treatment.
Torn ACL: Treatment methods with and without surgery (1/3)
(Dr. med. Andreas Krüger in interview with Rosanna Di Bello @blog.hirslanden.ch)
Knee injuries are the most frequent skiing accidents on the slopes, accounting for about 30% of all accidents. Right at the top of the statistics is the rupture of the cruciate ligament. There are various criteria that are taken into account when making individual decisions about treatment.
We were able to meet two patients of Dr. Andreas Krüger, attending physician at Klinik im Park and Klinik Hirslanden in Zurich. Both love skiing and both injured their anterior cruciate ligament. Their stories could not be more different. Former junior skier vs. hobby skier, surgery vs. conservative treatment.
How everything happened and which treatment was chosen can be found out in our two patient interviews:
Patient 1: "Torn ACL: I was treated conservatively without surgery"
Patient 2: "Torn ACL: I decided to have surgery"
In the following interview, Dr. med. Andreas Krüger explains to us why the torn cruciate ligament is a typical ski injury. At the same time, he explains when conservative and when operative treatment makes sense.
Dr. Krüger, we were pleased to meet two of your patients. Both suffered a cruciate ligament injury while skiing. What was surprising was the type of accident Mrs. Oehri had. A sporty young woman who fell over her own child in slow motion and tore her anterior cruciate ligament.
Does the athleticism of the person have an influence on the degree of cruciate ligament rupture injury?
Dr. Andreas Krüger: In many cruciate ligament ruptures, the athleticism (i.e. fitness) plays only a subordinate role. Decisive for the degree of injury are the accident mechanism and the force applied. Typical knee accidents when skiing happen not only on the piste, but also when standing in line at the lift, for example when a fall occurs with a fixed lower leg and the ski binding does not release.
Three mechanisms are frequently found:
The lower leg and the thigh are rotated against each other.
The knee experiences a x-leg malposition.
A combination to which the knee does not respond well with muscular stabilization.
In addition, it must be mentioned that mental and physical fatigue often has a significant influence on the degree of injury. In principle, accident rates are higher after lunch and on the last trip.
Is the torn cruciate ligament a typical skiing accident? Why is that?
Dr. Andreas Krüger: Skiing is one of the sports that puts a strain on the knees. Among skiers, both children and adults, the knee is the most frequently injured part of the body. According to the Swiss Council for Accident Prevention (bfu), around 69,000 skiers are injured on Swiss slopes every year, with around 1/3 of accidents involving the knee. The anterior cruciate ligament rupture with 38% of all knee injuries is the most frequently occurring specific diagnosis (Brucker et. al, Alpiner Skibreiten- und Skileistungssport, 2014).
Why this is so can be explained by the mechanism described above. Depending on the fall, the fixation of the lower leg and the rotation of the thigh can put a lot of strain on the knee and therefore also on the cruciate ligaments.
Is there anything that can be done before skiing to minimize the likelihood of injury?
Dr. med. Andreas Krüger: An essential factor is the preparation for the ski season and risk minimization. A well-trained musculature that knows when and how to function can help to reduce the probability of accidents in the risk area.
The right ski equipment and the correct adjustment of the binding by expert hands are actually a matter of course.
Two of your patients suffered a similar injury. But they chose different treatments. When is the surgical measure suitable, when the conservative measure?
Dr. med. Andreas Krüger: Whether a conservative or surgical measure is suitable for the patient depends on various criteria: biological age (how old does he feel), / actual age, presence of a meniscus injury, intensity of pain, sports practice (stop-and-go sports such as tennis, football or harmonious rhythmic movements such as swimming, golf), knee stability and last but not least the personal demands of the patient.
Crucial for the success of conservative treatment is the integrity of the meniscus and cartilage as well as the other ligaments in the knee. Recent studies have shown If the knee has a torn cruciate ligament as well as a meniscus and/or cartilage injury, the result is better if the knee is operated. The cruciate ligament is usually replaced by the body's own tendon. In this case, the operation also serves to protect the meniscus in order to avoid or minimise secondary diseases such as arthrosis, which is promoted by an additional meniscus injury.
That means in summary:
Good resilience directly after accident
Low performance requirements for the knee joint
No further injury to meniscus or cartilage
High requirement profile with stop-and-go sports, subjective instability
Additional injuries to meniscus, cartilage or other ligaments
Is one type of treatment less painful than the other?
Dr. med. Andreas Krüger: The surgical method is more painful directly after the operation only in individual cases, although this can be well controlled by modern anaesthetic procedures. Later, the course and symptoms are very similar.
What do you have to be aware of when you decide on one or the other measure?
Dr. med. Andreas Krüger: The Swiss Medical Board recommends treating cruciate ligament ruptures with conservative measures during the first three months, as there is a 30% chance that the cruciate ligament will heal without surgery. With good initial subjective knee stability, a knee joint that can be well loaded again without surgery can result. However, the factors time, muscular shrinkage and the risk of secondary meniscus injury with persistent instability must be considered. The secondary meniscus injury caused by the persistent knee instability is one of the most decisive factors for the long-term prognosis.
If the cruciate ligament does not heal during conservative treatment, secondary damage to the meniscus or cartilage may occur. In these cases, surgical treatment is also recommended.
According to the criteria of the international knee specialists, the recommendation for the surgical intervention is certainly the right decision for the patient Natalija Oehri.
How does the rehabilitation look like? Are there differences?
Dr. Andreas Krüger: The rehabilitation is divided into different phases.
In the first phase, the pain and swelling are mainly treated.
In the next phase, the focus is on promoting muscular stabilization.
The last phase is concerned with increasing the load on the knee. The knee is prepared specifically for the upcoming load. Before patients are allowed to resume their usual sports activities, they are subjected to the Ready-to-Sport test, in which at least 90% of the strength and stability of the uninjured opposite side must be achieved.
After the surgical treatment, walking sticks are used for three weeks to provide partial relief with full weight bearing in the extended position. With additional meniscus suture, the patient must relieve the load for four weeks and then gradually build up the load until the sixth week.
The non-surgical method requires a similar effort in physiotherapy, but the load is applied according to the complaints and swelling with permitted full load with the knee brace in place.
Torn cruciate ligament: Decision against surgery
Torn cruciate ligament: Decision against surgery. Patient (56 years old) fell while skiing and injured her knee. Diagnosis: Injury of the anterior cruciate ligament. From the beginning it was clear to her that surgical treatment was out of the question for her, provided there was an alternative, because every operation is associated with a certain risk. What happened in the accident, how she was treated and how she feels today, you will learn in the following interview.
Torn ACL: Treatment methods with and without surgery (3/3)
(Patient of Dr. med. Andreas Krüger in interview with Rosanna Di Bello @blog.hirslanden.ch)
"Torn ACL: I was treated conservatively without surgery"
Patient (56 years old) fell while skiing and injured her knee. Diagnosis: Injury of the anterior cruciate ligament. From the beginning it was clear to her that surgical treatment was out of the question for her, provided there was an alternative, because every operation is associated with a certain risk. What happened in the accident, how she was treated and how she feels today, you will learn in the following interview.
What does freedom of movement mean to you?
Patient: Freedom of movement is essential for me. Exercise and sports are part of my physical and mental well-being.
How much exercise do you do?
Patient: I do sports every week and I also like to do it in nature.
You were in a skiing accident, what happened?
Patient: During the downhill run in the afternoon, we always have a race within the family, with the winner usually being decided between my husband and our sons. We also did this on the day of the accident in the Grindelwald ski region. At first I tried to keep up and not lose the connection. But when there were a lot of people on the piste in narrow passages and I had to avoid a ski school class, I braked and drove to the edge of the piste. An edge fault, the higher snow and the greatly reduced speed caused me to crash. A burning pain on the inside of my right knee made me immediately fear that something must have torn.
Were you transported directly to the emergency?
Patient: No, a skier helped me up on my legs and I drove slowly to the valley station. My right leg was alarmingly unstable. I arrived at the bottom with a lot of concentration and caution. We then immediately sought medical help for first aid.
What treatment did the doctors give you?
Patient: The doctor in Grindelwald prescribed a soft protective splint and recommended cooling and elevation. I then went to Zurich myself for further treatment, which took place a week later in Dr. Krüger's practice. Dr. Krüger examined me and then showed me the MRI image of my cruciate ligament injury on the iPad. Seeing this image in front of me somehow took the horror out of me.
He introduced me to the various treatment options. I wanted to avoid an operation if possible and instead opt for conservative treatment with a splint, if this was really an option. I think Dr. Krüger noticed this very quickly and did not urge me to have an operation. When he then drew my attention to the fact that I would be given a thrombosis injection in the conservative treatment because of the restricted mobility, I knew that I wanted to have my known mobility back as quickly as possible. So on the same day I took care of a sports splint and made sure that I moved as much as possible.
How long did the rehabilitation (splint fitting / physiotherapy) last?
Patient: I felt excellent during the whole therapy and was cared for very professionally. For me, the knee injury also meant a sporting challenge. The therapy demanded a lot from me and made me aware of how important my freedom of movement and sports are to me.
The splint fitting lasted six weeks in principle and immediately gave me great mobility. However, I used the rail a little longer, as it did not restrict me at all and gave me protection and safety. The physiotherapy finally lasted almost a year, but I was much fitter afterwards than before the accident. After all, I wanted to go skiing again the following winter.
How long did it take to get you mobile again?
Patient: I was already mobile with the splint after two weeks. I could put full weight on the knee after three to four months. Hiking, golf and cycling were then back in fashion. However, I still had some pain and limitations, especially when doing sports with rotational movements like golf.
Did you underestimate anything in the healing process?
Patient: Yes, I underestimated myself! What was difficult for me was that I was totally decelerated. I love the faster sports and these were temporarily no longer possible. At the same time, it was a great experience to see how consistently and ambitiously I have personally committed myself to my body and my recovery. The physiotherapists helped me to heal myself successfully. I had not expected this experience.
How are you feeling today?
Patient: I feel very well and have no complaints in my knee. But that is mainly because I always do muscle training to protect my knees and my body in general. I run a lot and always take the stairs, so I build a little training into my everyday life.
Do you feel safe on skis again or do you still have a queasy feeling?
Patient: I feel as safe as before, I am not afraid and after the accident I live with the knowledge that skiing fast is much healthier for the knee than falling down in slow motion.
Cruciate ligament rupture: Decision for surgery
Cruciate ligament rupture: Decision to operate. Patient (37 years old), a sporty young mother of two sons, was about to teach her youngest son to ski when she fell in slow motion. She noticed immediately: There was something wrong with her knee. But the village doctor from the ski region assured her that everything was fine. 8 1/2 weeks later she decided to have the cruciate ligament operated. You can find out how it came about in the following interview.
Torn ACL: Treatment methods with and without surgery (2/3)
(Patient of Dr. med. Andreas Krüger in interview with Rosanna Di Bello @blog.hirslanden.ch)
"Torn ACL: I decided to have surgery"
Patient (37 years old), a sporty young mother of two sons, was about to teach her youngest son to ski when she fell in slow motion. She noticed immediately: There was something wrong with her knee. But the village doctor from the ski region assured her that everything was fine. 8 1/2 weeks later she decided to have the cruciate ligament operated. You can find out how it came about in the following interview.
What does freedom of movement mean to you?
Patient: Freedom of movement has always meant a lot to me. Until I was 19, I was in the junior skiing squad. I like to move around and I don't feel comfortable without regular sport.
How much exercise do you do?
Patient: During my career in the junior ski squad I trained either strength, endurance or speed five days a week. After my time in the squad I trained three times a week at home on my cross trainer. When the children came, two years followed in which I was no longer able to do sports as usual. But then the desire grabbed me again: cross-training at home, once a week on the tennis court and golfing every now and then. In winter I was found more regularly on the ski slopes again.
In the meantime I do strength exercises with my own body weight about three times a week instead of cross-training. The post-operative training after my operation has motivated me to do this.
You were in a skiing accident, what happened?
Patient: It happened on a family ski trip. My three-year-old son was wearing a so-called "Gstältli" and learned to ski. I held on to the straps and we went into a curve one after the other. My son fell and broke down. I was close behind him and braked abruptly. I caught the tip of my ski in the stem and it turned my right ski inwards. I felt a crack in my knee. I could already see myself lying on the operating table with a torn cruciate ligament and then limping around with crutches. After five minutes I gathered all my courage and stood up. Standing was possible without any problems. I had only slight pain. I just thought: Phew, lucky.
Were you transported directly to the emergency?
Patient: No, because I could still ski myself, we then went to the middle station in the ski area and took the chair lift to the valley station. To be on the safe side, I went to the village doctor and showed him my knee. But he more or less smiled at me and said that everything was fine. Relieved by his diagnosis, I went about my usual daily routine: playing tennis regularly and riding my bike to work. Although I was in slight pain, I didn't think anything of it.
After about two months of constant pain, I found the whole thing quite astonishing and went to a specialist to have my knee examined again. After a short examination of my knee, the diagnosis was clear for him, contrary to the village doctor's diagnosis: a torn anterior cruciate ligament. The very next day I had an MRI examination which confirmed his diagnosis.
What treatment have you had?
Patient: Dr. Krüger informed me very neutrally about the treatment options. I was uncertain whether I should decide for or against an operation. I expressed my concerns to Dr. Krüger and emphasized that it was important for me to be able to pursue my hobbies again without any problems, especially skiing and playing tennis. Dr. Krüger explained to me that in my case an operation was the better solution. Today I am sure that I have made the right decision.
How did you feel after the operation?
Patient: I had severe pain the first few days and found it very unpleasant that the knee could neither be straightened nor properly bent. In addition, I was often nauseous from the anesthesia and medication.
How long did the rehabilitation (splint fitting / physiotherapy) last?
Patient: On the second day after the operation I was able to get up again and go to the toilet on my own. From the first day on, I trained three times a day with the knee movement splint, the electrodes for muscle building and from the second day on, regular physiotherapy was added.
I wore the splint for about two months, it gave me a certain security. I went to physiotherapy once or twice a week for six months.
How long did it take to get them mobile again?
Patient: The swelling in the knee unfortunately did not go down as quickly as hoped. When we went on holiday to the sea six weeks after the operation, I was still using crutches and could not yet put full weight on them. The two weeks on the beach and the salt water did me good. When I returned to Switzerland, i.e. eight weeks after the operation, I was able to walk without crutches, put full weight on them and drive a car again without any problems.
Did you underestimate anything in the healing process?
Patient: The only difficulty was the demanding and strict physiotherapy, which I appreciated very much. I think the only reason I feel so well today is because my therapist regularly pushed me to my limits.
Taping in sports and rehabilitation
Since the European Football Championship in 2012 at the latest, we have known what tape is in sport. Muscles tensed to the max, a petrified gaze - the pose of Mario Balotelli after his 2-0 victory over Germany in the semi-finals. Bare perfectly trained upper body. This winner pose has immediately etched itself into the collective memory of European Championship spectators worldwide. But how much effect is really hidden in these audience-effective, glued-on, brightly coloured tapes? More power, less pain, more precision and faster recovery after exhausting competitions?
Effective use of taping in polo sport
(Andreas Krüger MD @Poloplus10.com)
Since the European Football Championship in 2012 at the latest, we have known what tape is in sport. Muscles tensed to the max, a petrified gaze - the pose of Mario Balotelli after his 2-0 victory over Germany in the semi-finals. Bare perfectly trained upper body. This winner pose has immediately etched itself into the collective memory of European Championship spectators worldwide. But how much effect is really hidden in these audience-effective, glued-on, brightly coloured tapes? More power, less pain, more precision and faster recovery after exhausting competitions?
The success of this method has lasted for over 30 years. In 1979, the Japanese Dr. Kenzo Kase had the brilliant pioneering idea of supporting his chiropractic treatment with elastic cotton tapes and prolonging its effect. Dr. Kase began his tape therapy for sumo wrestlers using skin-coloured adhesive tapes that were modelled on the texture of the skin. The finely woven, breathable and highly elastic cotton is glued with tension to affected parts of the body. This is intended to cause additional displacement of the skin layers, as the skin is slightly lifted by the movement and the pressure on the pain receptors in the lower skin layer is reduced. The visually appealing application technique is intended to trigger a stimulating effect on the muscles. According to the manufacturer (whose names are manifold), an additional effect of the increased blood circulation and the resulting supported drainage of lymph fluid are the result and serve for better regeneration.
The study situation in the electronic medical world literature (Pubmed) currently shows no uniformly significant results regarding the sustained effect of different tape variants. There are, however, case reports that have demonstrated the tendency for improvements in strength and pain in athletes of different colours.
In the sport of polo, injuries to the muscles and the tendons and ligaments of the beating arm regularly occur due to excessive strain. Punches of the opponent in hot duels as well as the frequent falls leave painful injuries. Also back problems during the powerful blows in an otherwise unfamiliar position over the neck of the pony take their toll due to the maximum strain on the body. Within a tournament, the elastic tapes can be applied to stabilize the shoulder and the player can continue to play without shoulder dislocation. Even after the stroke on the thumb of the batting arm, the swelling can be supported by applying the tape in a lymph drainage stimulating way. In the last chukker, when strength becomes the decisive factor, upper arm or forearm taping can influence the player's condition. A stabilising tape can also be helpful in the case of acute knee injuries.
Polo player Andres "Lala" Laplacette is delighted with the effect of the tapes: "I tried the tapes for the first time at the Arena Polo World Cup Azerbaijan in Baku. There I had injured my back very painfully. Before that, I had seen similar tapes with other athletes and wondered if they could help me. I tried the tapes and felt relieved. It was as if someone was holding my back muscles. Additionally, they were warmed by the tapes. I could continue the game without any problems. I was overjoyed because being in Baku for the first polo tournament was a great opportunity for all of us. On the last day of the tournament, Dr. Krüger placed a tape on my arm, because I was hurting all over. I would have loved to have the tape all over my body!"
Tapes also helped Tito Gaudenzi (polo player) a lot: "In polo we are exposed to many abrupt and extreme movements. It's the nature of the sport: the speed, the riding, the playing. Especially the back and shoulders suffer from it. Tapes can quickly improve these problems. Applied before the game, they stabilize and improve mobility. At one of my last tournaments in Baku, I had severe pain in my lumbar region from a previous injury. Dr. Andreas Krüger helped me to get fit again for the match. The right work-out before the match and especially the correct taping allowed me to continue fighting. I can highly recommend taping for all kinds of sports. It's a simple and yet very effective solution."
So the conclusion is that modern science cannot prove it - but are Mario Balotelli, Serena Williams and David Beckham wrong? In any case, they have achieved their sporting achievements.
Summarized advantages of taping
Muscle activation
Restoration of the injury
Edema control (reduction of swelling)
Posture correction
Pregnancy support
Support for sporting and athletic performance
Sports Taping
Athletic taping is recognized as one of the top preventative measures for reduction of injuries in collision sports. Taping was popularised by Dr. Kenzo Kase, who officially developed the Kinesio Taping Method in 1979 Using Sports Taping can give you the security you need to stay on the field and avoid those niggling injuries.
Effective use of taping in the sport of polo
(Andreas Krüger MD @Poloplus10.com)
We know about taping in sport since the 2012 European Football Championship at the latest. The muscles maximum tense, with a stony look - the posture of Mario Balotelli in the semi-final against Germany after making it 2-0. Bare, perfectly trained chest. This winning pose immediately burned itself into the spectator's minds. But what effects do these catchpenny, affixed and gaudily coloured tapes really have? More strength, less pain, more precision and a rapid recovery after exhausting competitions?
The success of this method lasts for more than 30 years. In 1979, the Japanese Dr. Kenzo Kase had the dazzling idea to support and extend the effect his chiropractic therapy by use of elastic cotton tapes. Dr. Kase started his tape therapy with sumo wrestlers by use of skin-coloured tapes, which are based on the consistency of the skin. The finely woven, breathable and highly elastic cotton is glued with tension on affected body locations. Through this, an additional shift of the layers of skin is supposed to take place, because through the movement the skin is being lifted and the pressure on the pain receptors in the lower layers of skin is being reduced. A stimulating effect for the muscles is meant to be induced through the visual appealing technique of application. According to the producers, an additional effect of the heightened circulation and the hereby supported drain of lymph fluid are a consequence of this and conduce to a better regeneration.
The scientific findings in the electronic medical world literature (Pubmed) currently show no consistent, significant results regarding the enduring effect of different tape variants. But case reports exist which achieved to prove the tendential improvement through different applications of the tapes regarding strenght and pain of the athletes of all shades.
In the sport of Polo, injuries of the muscles as well as of the sinews and ligaments of the arms which beat the ball develop regularly due to excessive stress. Strikes of the opponent during a tackling as well as the not uncommon downfalls leave painful injuries. Back complaints as a result of strong strikes in an unusual position over the neck of the pony also take a toll on the players due to the maximum strain of the body. During a tournament the applications of the elastic tapes can accomplish a stabilisation of the shoulder and the player can finish the match without a dislocation of the shoulder. Even after a blow on the thumb of the arm which beats the balls the application of a tape can support the detumescence through the drain of the lymph fluid. In the last chukker, when strength becomes the decisive factor, the condition of the player can be influenced by tapings of the upper arm and the forearm. The stabilising tapes can also be helpful at acute knee injuries.
Polo player Andres "Lala" Laplacette is excited about the effect of the tapes: "I tried the tapes for the first time in Baku (during the Arena Polo World Cup Azerbaijan). I fell on my back, and it was hurting quite bad! I had seen similar tapes before on other athletes and I was wondering whether they could help me or not. After trying them I felt more relieved. On the one side it seems like somebody was holding the muscles of my back. And on the other side, the tapes were keeping them warm. I could play the rest of the games with no problem! I was really happy because it was a big opportunity for all of us to play polo there for the first time. On the last day the Dr. Krüger placed me one on my arm, because after two games on the days before, everything was hurting. So I would have liked tapes all over my body!
The tapes also helped Tito Gaudenzi (polo player) a great deal: "I have had a great experience with tapping in my sport. In Polo we are exposed to a lot of abrupt and extreme movements given the nature of the sport, the speed, riding the horse and playing the game. "A lot of common issues are back and shoulder problems. Both can rapidly be improved by taping it the right way before the game. It gives it more stability and increasing movement. In one of my last tournaments in Baku, Azerbaijan I had experienced some severe lower back pain from a prior injury. Dr. Andreas Krüger helped me be ready for the game through the right pre-game work out and most importantly the correct tapping that allowed me to successfully compete again. I can only strongly recommend taping in my sport or any other. Its a simple and effective solution that can easily be applied if and when done correctly.
In summery, it can be said, therefore, that modern science cannot prove it - but are Mario Balotelli, Serena Williams and David Beckham off the base? In any case they have delivered their sporting performances.
Summarized benefits of taping
Pain relief
muscle activation
Injury recovery
Oedema control (swelling reduction)
Postural correction
pregnancy support
Assisting athletic & sports performance